Dental care is a critical aspect of overall health, but for many Americans, accessing affordable services can be a challenge. Medicaid, the government-funded health insurance program for low-income individuals and families, provides dental coverage, but understanding the intricacies of this program can be daunting. This guide delves into the world of Medicaid dental insurance, exploring eligibility criteria, coverage benefits, enrollment procedures, and essential resources.
From understanding the specific procedures covered to navigating the enrollment process and finding participating providers, this comprehensive overview aims to empower individuals to make informed decisions about their dental care. We will also shed light on common misconceptions, alternative options for those ineligible for Medicaid, and the evolving landscape of dental coverage for this population.
Eligibility Criteria
Medicaid dental insurance is a government-funded program that provides dental coverage to low-income individuals and families. To be eligible for Medicaid dental insurance, individuals must meet certain income and asset limitations, age requirements, and residency requirements. Additionally, certain medical conditions may qualify individuals for Medicaid dental insurance.
Income and Asset Limitations
To qualify for Medicaid dental insurance, individuals must meet specific income and asset limitations. These limitations vary by state and are based on the Federal Poverty Level (FPL). The FPL is a measure of poverty used by the U.S. government to determine eligibility for certain programs, including Medicaid. For instance, a family of four with an annual income below 138% of the FPL may qualify for Medicaid dental insurance in some states.
In addition to income, individuals may also have asset limitations. These limitations may include restrictions on the value of a home, car, and savings accounts. For example, individuals may be required to have less than a certain amount of money in their bank accounts to qualify for Medicaid dental insurance.
It is important to note that income and asset limitations can vary significantly depending on the state. Individuals should contact their state’s Medicaid office for specific eligibility requirements.
Age Requirements
Medicaid dental insurance is generally available to children and adults who meet the eligibility criteria. However, some states may have specific age requirements for eligibility. For example, some states may provide dental coverage to children up to a certain age, such as 21.
States may also offer dental coverage to adults who are pregnant or breastfeeding, as well as adults with certain disabilities.
Residency Requirements
To be eligible for Medicaid dental insurance, individuals must be residents of the state in which they are applying for coverage. Residency requirements vary by state. Individuals should contact their state’s Medicaid office for specific residency requirements.
Specific Conditions
Individuals with certain medical conditions may be eligible for Medicaid dental insurance, even if they do not meet the standard income and asset limitations. These conditions may include:
- Pregnancy
- Breastfeeding
- Certain disabilities
- Certain chronic health conditions, such as diabetes and HIV/AIDS
Individuals with these conditions should contact their state’s Medicaid office to determine their eligibility for dental coverage.
Coverage Benefits

Medicaid dental plans provide essential oral healthcare services to eligible individuals. The specific benefits and limitations can vary depending on the state and the specific plan. However, most plans cover a range of services designed to prevent dental problems and address existing conditions.
Preventive Services
Preventive services are crucial for maintaining good oral health and preventing more serious dental issues. Medicaid dental plans typically cover these services, including:
- Dental cleanings (prophylaxis): Regular cleanings help remove plaque and tartar buildup, which can lead to cavities and gum disease.
- Dental exams (oral examinations): These exams allow dentists to assess the overall health of your teeth and gums, identify any potential problems, and provide necessary treatment recommendations.
- Fluoride treatments: Fluoride helps strengthen tooth enamel and protect against cavities, particularly in children.
- Dental sealants: Sealants are a protective coating applied to the chewing surfaces of back teeth to prevent cavities.
- X-rays (radiographs): X-rays provide a detailed view of the teeth and jawbone, allowing dentists to diagnose problems that may not be visible during a regular exam.
Restorative Services
When preventive measures are not enough, restorative services are needed to repair damaged teeth and restore oral function. Medicaid dental plans typically cover:
- Fillings (restorations): Fillings are used to repair cavities and restore the shape and function of damaged teeth.
- Crowns (caps): Crowns are used to cover and protect damaged or weakened teeth.
- Bridges: Bridges are used to replace missing teeth by anchoring artificial teeth to adjacent teeth.
- Root canals (endodontic therapy): Root canals are performed to treat infected or damaged tooth pulp.
- Extractions: Extractions are used to remove teeth that are severely damaged, decayed, or infected.
Other Covered Services
Medicaid dental plans may also cover additional services, such as:
- Dentures (complete or partial): Dentures are removable appliances that replace missing teeth.
- Oral surgery: Oral surgery includes procedures such as tooth extractions, bone grafts, and implant placement.
- Emergency dental care: Medicaid plans typically cover emergency dental services, such as pain relief and treatment for severe infections.
Limitations on Coverage
While Medicaid dental plans cover a wide range of services, there are some limitations to consider:
- Frequency of coverage: Some services, such as cleanings and exams, may have limits on how often they can be covered within a specific time period. For example, a plan might cover two cleanings per year.
- Specific procedures: Some procedures may not be covered by all Medicaid plans. For instance, some plans may not cover cosmetic dental work, such as teeth whitening or veneers.
- Prior authorization: Some services may require prior authorization from the Medicaid plan before they can be performed. This means you need to get approval from the plan before your dentist can proceed with the treatment.
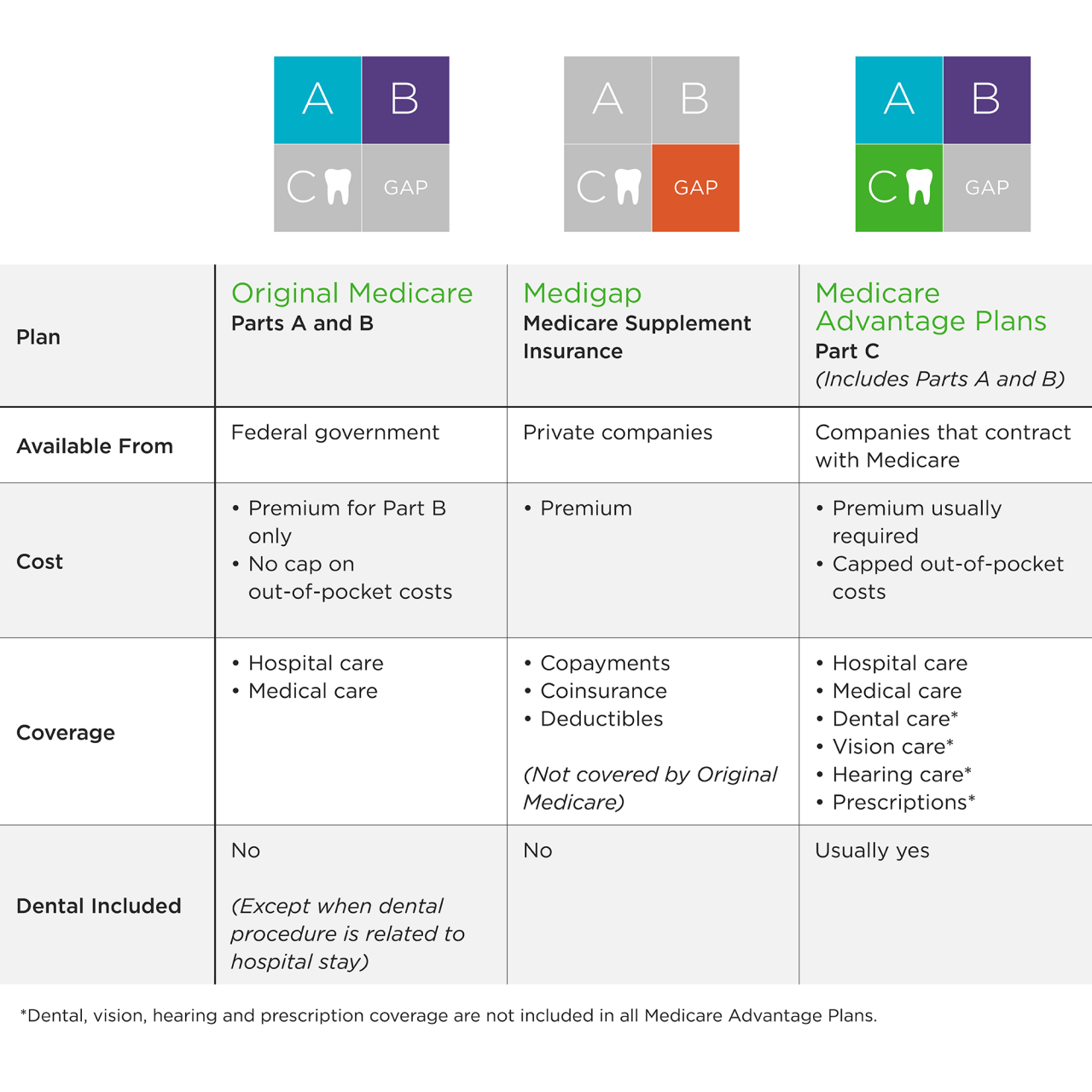
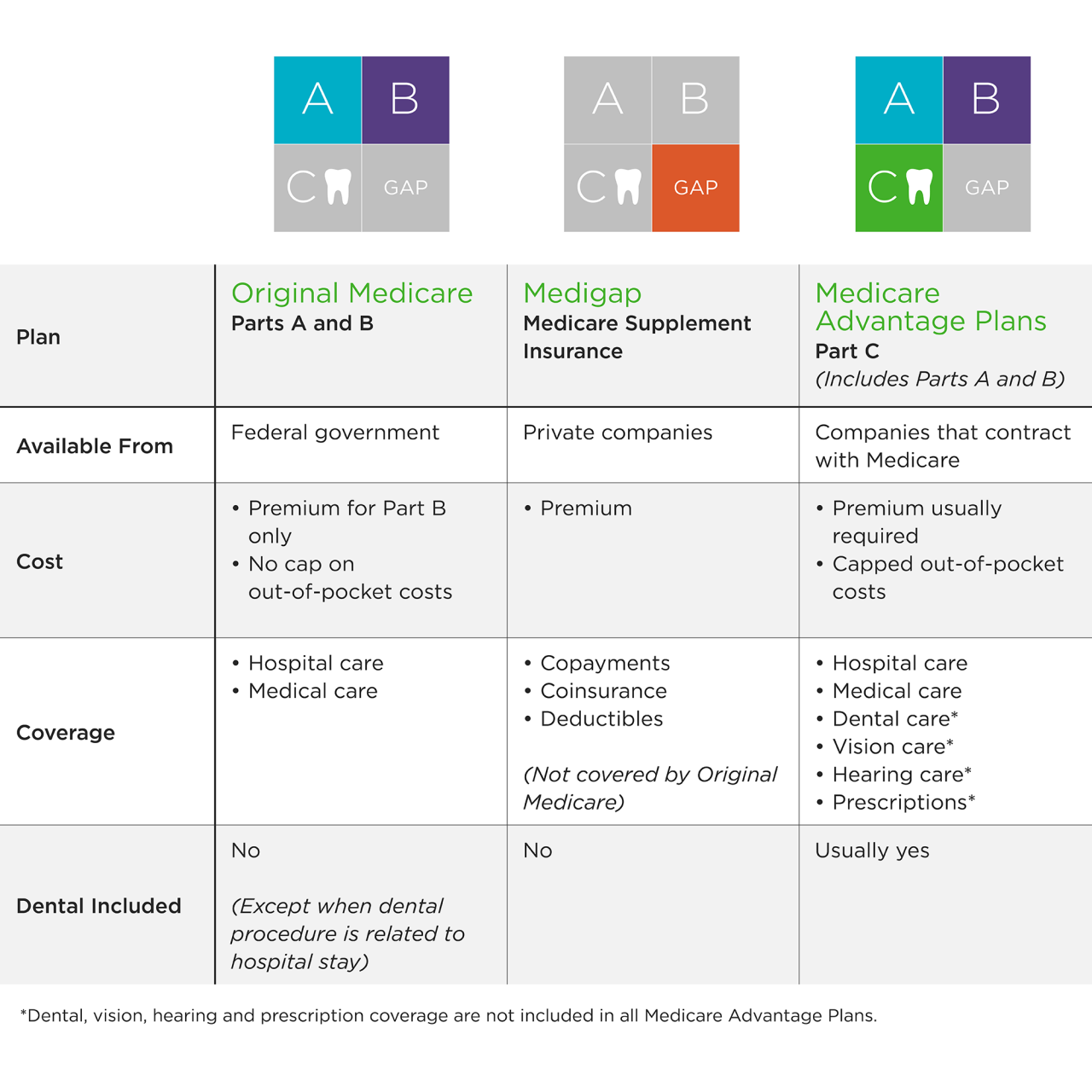
Comparing Medicaid Dental Plans
Medicaid dental plans can vary significantly in the benefits they offer. It’s important to compare different plans to find one that meets your individual needs. Factors to consider include:
- The range of services covered: Some plans may offer a wider range of services than others.
- Frequency limits: Check the frequency limits for specific services to ensure they meet your needs.
- Network of dentists: Ensure that the plan includes dentists in your area who accept Medicaid.
- Copayments and deductibles: Some plans may require copayments or deductibles for certain services.
Enrollment Process

Medicaid dental insurance enrollment is a straightforward process designed to provide access to essential dental care. This section will Artikel the steps involved, the necessary documentation, available enrollment channels, and the typical time frame for approval.
Required Documentation
To enroll in Medicaid dental insurance, you will need to provide specific documentation to verify your eligibility. This information helps ensure that you meet the program’s requirements and are entitled to receive benefits.
- Proof of identity, such as a driver’s license, state-issued ID card, or passport.
- Proof of residency, such as a utility bill, lease agreement, or bank statement.
- Proof of income, such as pay stubs, tax returns, or unemployment benefits documentation.
- Social Security number for all household members.
- Proof of citizenship or legal residency, such as a birth certificate, naturalization certificate, or green card.
- In some cases, you may also need to provide documentation related to your disability, pregnancy, or other qualifying factors.
Application Process
The application process for Medicaid dental insurance involves submitting the required documentation and completing a comprehensive application form.
- Online Application: Many states offer online application portals for Medicaid dental insurance. This option allows you to conveniently complete the application and submit it electronically, typically through the state’s official website.
- Phone Application: You can also apply for Medicaid dental insurance by phone. Call the Medicaid office in your state to request an application form and receive assistance with the process.
- In-Person Application: If you prefer, you can apply for Medicaid dental insurance in person at a local office or designated enrollment center. You can find the nearest location by contacting your state’s Medicaid agency.
Enrollment Approval Time Frame
Once you submit your application and required documentation, the Medicaid agency will review your information to determine your eligibility. The processing time for approval can vary depending on the state and the complexity of your application.
On average, it may take 30 to 60 days to receive a decision on your application.
Provider Networks
Medicaid dental insurance programs typically have a network of participating dental providers. This network includes dentists, dental hygienists, and other dental professionals who have agreed to provide services to Medicaid beneficiaries at a discounted rate.
Participating Dental Offices
The participating dental offices in the Medicaid network vary depending on the state and the specific Medicaid plan. However, most plans include a wide range of dental providers, including general dentists, specialists such as orthodontists and oral surgeons, and dental hygienists. To find a specific provider within the network, you can use the following resources:
- Your state’s Medicaid website: Most state Medicaid websites have a provider directory that allows you to search for participating dental offices by location, specialty, and other criteria.
- The Medicaid managed care plan’s website: If you have a Medicaid managed care plan, you can also find a provider directory on their website.
- The National Committee for Quality Assurance (NCQA): The NCQA provides a directory of accredited dental providers, including those who participate in Medicaid programs.
Cost and Payment
Medicaid dental insurance covers a wide range of dental services, including preventive care, restorative treatments, and emergency procedures. While the program is designed to provide affordable dental care, there are some costs associated with it. This section will discuss the costs associated with Medicaid dental insurance, including co-payments, deductibles, and financial assistance.
Co-payments and Deductibles
Co-payments and deductibles are common features of most health insurance plans, including Medicaid dental insurance. They are designed to share the cost of dental care between the patient and the insurance provider.
- Co-payments are fixed amounts that Medicaid recipients may be required to pay at the time of service. The amount of the co-payment may vary depending on the specific service received and the state’s Medicaid program.
- Deductibles are the amount that Medicaid recipients must pay out-of-pocket before the insurance coverage kicks in. Once the deductible is met, the insurance will cover a portion of the remaining costs.
Payment Process
The payment process for covered dental services under Medicaid typically involves the following steps:
- The Medicaid recipient receives dental services from a participating provider.
- The provider submits a claim to the Medicaid program for reimbursement.
- Medicaid reviews the claim and processes payment to the provider.
- The Medicaid recipient may be responsible for paying any co-payments or deductibles at the time of service.
Financial Assistance
For Medicaid recipients who may struggle to afford even the co-payments and deductibles associated with dental care, there are several financial assistance options available.
- State-funded programs: Some states offer additional financial assistance programs to help Medicaid recipients with dental care costs. These programs may provide grants or subsidies to cover co-payments, deductibles, or even the full cost of dental services.
- Dental schools and clinics: Dental schools and clinics often offer discounted dental care to low-income individuals and families, including Medicaid recipients.
- Community health centers: Many community health centers provide affordable dental care to underserved populations, including Medicaid recipients.
Dental Health Resources
Maintaining good oral health is crucial for overall well-being. Medicaid recipients have access to various resources that can help them achieve and maintain a healthy smile.
Dental Care Services
These resources provide access to a wide range of dental care services, from routine checkups to more complex procedures.
- Find a Dentist: The Medicaid website or your state’s dental program website provides a directory of dentists who accept Medicaid. This allows you to locate a dentist near you who is in your network.
- Community Health Centers: Many community health centers offer dental care services to low-income individuals and families, including Medicaid recipients. These centers often have sliding-scale fees based on income and may provide financial assistance.
- Dental Schools: Dental schools often have clinics that offer discounted or free dental care to patients as part of their training programs. This can be a good option for those who need more extensive dental work.
- Non-profit Organizations: Numerous non-profit organizations provide dental care services to underserved communities, including Medicaid recipients. These organizations may offer free or low-cost dental care, depending on their resources and the individual’s needs.
Dental Health Education
Dental health education plays a vital role in promoting good oral hygiene practices.
- Online Resources: The American Dental Association (ADA) and other organizations offer comprehensive online resources on dental health, including information on brushing, flossing, and other preventive measures.
- Community Outreach Programs: Many organizations conduct community outreach programs to educate the public about dental health. These programs may include presentations at schools, community centers, and other public venues.
- Dental Professionals: Dentists and hygienists provide valuable information on dental health during routine checkups and cleanings. They can offer personalized advice on oral hygiene practices and answer any questions you may have.
Preventative Dental Care
Preventative dental care is essential for maintaining oral health and preventing dental problems.
“Regular dental checkups and cleanings can help detect and address dental issues early on, reducing the need for more complex and costly treatments later.”
- Brushing and Flossing: Brushing twice a day with fluoride toothpaste and flossing daily removes plaque and bacteria, preventing cavities and gum disease.
- Regular Checkups: Visiting your dentist for regular checkups and cleanings allows them to identify and address any potential problems before they become serious.
- Healthy Diet: Limiting sugary drinks and snacks and consuming a balanced diet rich in fruits, vegetables, and whole grains can help prevent tooth decay.
Common Misconceptions
Medicaid dental insurance, like any insurance plan, is often subject to misconceptions. Understanding the nuances of coverage and limitations is crucial for maximizing benefits and avoiding disappointment. This section addresses common misconceptions and clarifies important aspects of Medicaid dental insurance.
Coverage Limitations
Medicaid dental insurance, while providing essential dental care, has specific coverage limitations. These limitations are designed to ensure responsible utilization of resources and prioritize the most critical dental needs.
- Limited Coverage for Cosmetic Procedures: Medicaid generally does not cover cosmetic dental procedures such as teeth whitening or veneers, focusing primarily on restorative and preventive care.
- Pre-authorization Requirements: Certain dental procedures may require pre-authorization from the Medicaid program. This process involves obtaining approval before the procedure is performed, ensuring that the service is medically necessary and within the coverage guidelines.
- Limited Coverage for Orthodontics: Orthodontic treatment, such as braces, is often subject to specific criteria and limitations under Medicaid. Coverage may be restricted to individuals with certain medical conditions or developmental issues requiring orthodontic intervention.
Provider Network Restrictions
Medicaid dental insurance typically operates within a defined network of providers. This network consists of dentists who have agreed to accept Medicaid payment rates for their services.
- Limited Provider Choice: Individuals enrolled in Medicaid dental insurance may have a more limited choice of dentists compared to private insurance plans. The network of providers may not include all dentists in a particular geographic area.
- Importance of Verifying Network Participation: It is essential to verify that a chosen dentist is part of the Medicaid network before scheduling an appointment. This ensures that the dentist will accept Medicaid payment for services rendered.
- Potential for Out-of-Network Costs: Seeking dental care from a provider outside the Medicaid network can result in higher out-of-pocket costs. Individuals are generally responsible for the difference between the Medicaid payment rate and the provider’s full fee.
Importance of Accurate Information
Obtaining accurate information from reliable sources is essential to dispel misconceptions and make informed decisions about dental care.
“It’s crucial to consult official Medicaid websites, dental provider websites, and reputable health organizations for accurate information about coverage, benefits, and limitations.”
- Official Medicaid Website: The official Medicaid website for the specific state provides comprehensive information about dental coverage, eligibility criteria, and provider networks.
- Dental Provider Websites: Many dental providers have dedicated sections on their websites outlining their participation in Medicaid programs and any specific coverage details.
- Reputable Health Organizations: Organizations like the American Dental Association (ADA) and the National Association of Dental Plans (NADP) provide valuable resources and information about dental insurance and coverage.
Real-Life Experiences
Understanding real-life experiences can provide valuable insights into the practical aspects of Medicaid dental insurance.
- Case Study: Limited Coverage for Dentures: A patient with dentures needing replacement discovered that Medicaid coverage for dentures is often limited to a specific timeframe or number of replacements. This highlights the importance of understanding coverage limitations and exploring alternative options for denture care.
- Case Study: Pre-authorization Process: A patient needing a complex dental procedure encountered a pre-authorization requirement, delaying the treatment until approval was obtained. This emphasizes the importance of understanding the pre-authorization process and allowing sufficient time for approval.
Alternative Options

For individuals who do not qualify for Medicaid, exploring alternative dental insurance options is crucial. Fortunately, several programs and plans cater to low-income individuals, ensuring access to essential dental care.
Affordable Dental Plans
Many dental insurance plans offer affordable options for low-income individuals. These plans may have lower premiums and deductibles, making them accessible to those with limited budgets.
Factors to Consider When Choosing an Affordable Dental Plan
- Coverage Benefits: Evaluate the specific services covered, such as cleanings, fillings, and extractions, and any limitations on coverage.
- Premium Costs: Compare monthly premiums and consider the plan’s overall cost-effectiveness.
- Deductibles and Co-pays: Understand the out-of-pocket expenses you’ll be responsible for before coverage kicks in.
- Provider Network: Ensure the plan includes dentists in your area and those you prefer.
Government-Sponsored Programs
The Children’s Health Insurance Program (CHIP) provides affordable health insurance coverage for children in families who do not qualify for Medicaid. CHIP offers comprehensive dental benefits, including preventive care, restorative treatments, and emergency services.
Dental Care Assistance Programs
Many organizations and charities offer dental care assistance programs to low-income individuals. These programs may provide financial assistance for dental procedures, access to free or discounted dental care, or connections to volunteer dentists.
Finding Dental Care Assistance Programs
- Local Health Departments: Contact your local health department for information on available programs and resources.
- Community Health Centers: Many community health centers offer dental services on a sliding-fee scale based on income.
- Dental Schools: Dental schools often provide discounted or free dental care as part of their training programs.
- National Organizations: Organizations like the American Dental Association (ADA) and the National Association of Dental Plans (NADP) can provide resources and information on dental care assistance programs.
Future Trends
The landscape of Medicaid dental insurance is constantly evolving, driven by factors such as changing demographics, technological advancements, and evolving healthcare policy. These developments are shaping the future of dental care access for Medicaid recipients, presenting both challenges and opportunities.
Impact of Healthcare Trends on Dental Coverage
The increasing focus on preventative care and chronic disease management within the broader healthcare system is influencing dental coverage as well. This shift is encouraging the integration of oral health into overall health, emphasizing the link between oral health and systemic health. As a result, Medicaid dental programs are likely to see an expansion of preventative services, including routine checkups, cleanings, and fluoride treatments, to reduce the incidence of dental problems and their associated health complications.
Conclusion
Navigating the complex world of Medicaid dental insurance can be challenging, but armed with the right information, individuals can access the care they need. Understanding eligibility criteria, exploring coverage benefits, and familiarizing oneself with the enrollment process are crucial steps towards securing affordable and comprehensive dental care. By embracing preventive measures, seeking out available resources, and staying informed about future trends, individuals can take control of their oral health and build a brighter smile.